The relationship between BIM deletion polymorphism and clinical significance of epidermal growth factor receptor-mutated non-small cell lung cancer patients with epidermal growth factor receptor-tyrosine kinase inhibitor therapy: a meta-analysis
Introduction
Lung cancer is the most common morbidity and mortality cancer all over the world. About 89% of lung cancer patients are non-small cell lung cancer (NSCLC) (1), and when patients were diagnosed as NSCLC, most lost chance to have surgery or radical resection, the only treatment is chemotherapy which only can extend a little time to live and the side effects are critical (2). When the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) such as gefitinib and erlotinib come out, the NSCLC patients who have an activating mutation of the EGFR gene have a new method to treatment, which can longer progression-free survival (PFS) than did those who received platinum-based chemotherapy, while also improving quality of life (3). However, the efficacy of EGFR TKIs cannot stay for long, about 10 to 16 months to develop a recurrence (4). The mechanism of resistance to EGFR-TKIs is not sure, it includes the acquisition of the T790M gatekeeper mutation, kinase switching due to mesenchymal-epithelial transition (MET) amplification, phosphatidylinositol-4,5-bisphosphate 3-kinase, catalytic subunit alpha (PIK3CA) mutation, and transformation into small-cell lung cancer (5-7).
B-cell lymphoma-2-like 11 gene (BIM), a member of the B-cell lymphoma-2 (Bcl-2) family genes, encodes BCL-2 interaction mediator of cell death protein (BIM), which is a critical modulator in promoting cell apoptosis (8). The impaired expression of pro-apoptotic BCL2-homology domain 3 (BH3) because of a 2903-bp germline deletion polymorphism of BIM, can be considered as an impossible factor cause the resistance of EGFR TKIs in EGFR-mutated NSCLC patients (9).
There are many trials focus on the relationship between BIM deletion polymorphism and EGFR-mutated patients accepted EGFR-TKIs for therapy.
It is still unclear whether the efficacy of EGFR-TKIs for NSCLC was associated with BIM polymorphism status in EGFR mutant patients. The aim of this meta-analysis was to summarize all the available evidence and determine the predictive role of BIM deletion polymorphism for EGFR-TKIs in NSCLC.
Materials and methods
The studies were found on PubMed and the Web of Knowledge databases dating up to July, 2015. The searching key words include “BIM deletion polymorphism”, “EGFR-TKI and BIM”, and “EGFR-TKI and polymorphism”. Study selection was based on an initial screening of identified abstracts or titles and a second screening of full-text articles. Eligible studies were identified from relevant full-text study in accordance with the following inclusion criteria: (I) the study focus on BIM deletion polymorphism and EGFR-TKI treatment; (II) patients must be detected to find whether have BIM deletion polymorphism; (III) the patients in the study must have EGFR-mutate and receive EGFR-TKIs as a major treatment; (IV) studies quantified outcomes with adjusted odds ratios (OR), relative risk (RR), hazard ratio (HR), or number of events and corresponding 95% confidence intervals (CIs); (V) published full text available.
OR, HR, and 95% CI was used as common measurements for evaluating the strength between BIM deletion polymorphism and survival as well as response to EGFR-TKI therapy in lung cancer patients. All calculations were performed using Revman5.3 (The Nordic Cochrane Centre, the Cochrane Collaboration, Copenhagen, Denmark).
Results
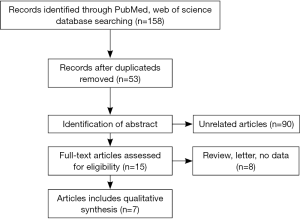
A total of 159 relevant studies were retrieved and searched in the databases and manual retrieval. A total of 41 duplicated articles; 103 unrelated articles; and eight reviews, letter, or no data including were excluded from the present study in accordance with inclusion and exclusion criteria. As a result, seven eligible studies concerning BIM polymorphism and clinical response and outcome of EGFR-mutated NSCLC with EGFR-TKI treatment were selected in the meta-analysis (10-15). The flow chart of eligible study search was shown in Figure 1.
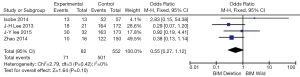
The relationship between BIM deletion polymorphism and the clinical outcome of EGFR-TKI in EGFR-mutated NSCLC patients were evaluated by combing with four original studies. Significant association was found between BIM deletion polymorphism and efficacy of EGFR-TKI treatment in patients (OR =0.55, 95% CI, 0.33−0.92) (Figure 2). And the disease control rate (DCR) in patients with BIM deletion polymorphism was decreased compared with patients without BIM deletion polymorphism (OR =0.55, 95% CI, 0.27−1.12) (Figure 3).

Six eligible studies reported association between BIM deletion polymorphism and PFS in EGFR-TKIs treated NSCLC patients. And the result was showed in Table 1. The PFS of patients with BIM deletion polymorphism was shorter than those patients with BIM wild type.
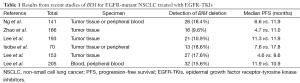
Full table
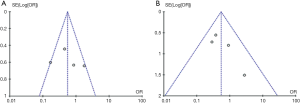
Results of Begg’s funnel plot showed that no significant publication bias was found between objective response rate (ORR), DCR, and BIM polymorphism, respectively. There was no significant publication bias in comparison of BIM deletion and BIM wild type in ORR and DCR (Figure 4).
Discussion
EGFR-TKIs have been a new treatment on NSCLC patients with EGFR mutation, which can longer patients living time and decrease the side effects. However, a large number of NSCLC patients harbored EGFR mutation displayed primary resistance to EGFR-TKIs (6). BIM deletion polymorphism is a germline that affects EGFR-TKI related apoptosis, which might lead to less or no BH3 expression. Therefore, a common deletion polymorphism within BIM was deemed as a candidate genetic cause of intrinsic resistance to kinase inhibitor therapy in these malignancies (10).
In order to make out the relationship between BIM deletion polymorphism and the clinical outcome in EGFR-mutated NSCLC patients received EGFR-TKIs, a meta-analysis was conducted by combing the data of eligible studies. Our results indicated that BIM deletion polymorphism contributed to a lower ORR and DCR in NSCLC patients than patients with BIM wild type treated with EGFR-TKIs. In addition, EGFR-mutated NSCLC patients who harbored BIM deletion polymorphism had a short PFS as compared to patients with BIM wildtype, showing that BIM deletion polymorphism may be a poor prognostic factor for EGFR-mutated NSCLC patients with EGFR-TKIs therapy. The deletion polymorphism is a 2,903 bp fragment deletion locus which is located in intron 2 and its frequency is only in Asian population, but absent in African and North American populations (10,16,17). BIM upregulation is required for TKIs to induce apoptosis in kinase-driven cancers through encoding a BH3-only protein which is a BCL2 family member (18). The BH3-only protein activated cell death by opposing the prosurvival members of the BCL2 family or by binding to the pro-apoptotic BCL2 family members and activating their pro-apoptotic functions (10). The polymorphism switched BIM splicing from exon 4 to exon 3 which caused the BIM lacking the crucial BH3 domain (19). That leads to the lower responses to TKI than do individuals without the polymorphism. This may be the cause why BIM deletion polymorphism was associated with poor clinical outcome in EGFR-mutated NSCLC patients with TKI targeted therapy (20).
However, because the difficulty of follow-up, only about two studies offered the overall survival (OS) of patients, we cannot evaluate the influence of BIM deletion polymorphism on the EGFR-mutated NSCLC patients received EGFR-TKI. And eligible studies were a few and were only searched on the databases of the Web of Knowledge and the PubMed. Then the sample was not big enough.
In summary, BIM deletion polymorphism was associated with poor RR, DCR, PFS in EGFR-mutated NSCLC patients received EGFR-TKI. Which indicated it might be a genetic cause of intrinsic resistance to TKI therapy in EGFR-mutated NSCLC and it could be emerged as an independent predictive biomarker to identify patients who would benefit from TKI targeted therapy in EGFR-mutated NSCLC.
Acknowledgements
Funding: This study was supported by the Natural Science Foundation of Jiangsu Province (No. BK2011658), Clinical Science and Technology Project of Jiangsu Province (No. BL2013026) and the National Natural Science Foundation of China (No. 81302032, No. 81572937, No. 81572273).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin 2014;64:9-29. [PubMed]
- Lee CB, Stinchcombe TE, Rosenman JG, et al. Therapeutic advances in local-regional therapy for stage III non-small-cell lung cancer: evolving role of dose-escalated conformal (3-dimensional) radiation therapy. Clin Lung Cancer 2006;8:195-202. [PubMed]
- Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42. [PubMed]
- Ciardiello F, Tortora G. EGFR antagonists in cancer treatment. N Engl J Med 2008;358:1160-74. [PubMed]
- Jung SK, Lee MH. Isoliquiritigenin induces apoptosis and inhibits xenograft tumor growth of human lung cancer cells by targeting both wild type and L858R/T790M mutant EGFR. J Biol Chem 2014;289:35839-48. [PubMed]
- Cappuzzo F, Jänne PA, Skokan M, et al. MET increased gene copy number and primary resistance to gefitinib therapy in non-small-cell lung cancer patients. Ann Oncol 2009;20:298-304. [PubMed]
- Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3:75ra26. [PubMed]
- Gillings AS, Balmanno K, Wiggins CM, et al. Apoptosis and autophagy: BIM as a mediator of tumour cell death in response to oncogene-targeted therapeutics. FEBS J 2009;276:6050-62. [PubMed]
- Faber AC, Corcoran RB, Ebi H, et al. BIM expression in treatment-naive cancers predicts responsiveness to kinase inhibitors. Cancer Discov 2011;1:352-65. [PubMed]
- Ng KP, Hillmer AM, Chuah CT, et al. A common BIM deletion polymorphism mediates intrinsic resistance and inferior responses to tyrosine kinase inhibitors in cancer. Nat Med 2012;18:521-8. [PubMed]
- Lee JK, Shin JY, Kim S, et al. Primary resistance to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) in patients with non-small-cell lung cancer harboring TKI-sensitive EGFR mutations: an exploratory study. Ann Oncol 2013;24:2080-7. [PubMed]
- Lee JH, Lin YL, Hsu WH, et al. Bcl-2-like protein 11 deletion polymorphism predicts survival in advanced non-small-cell lung cancer. J Thorac Oncol 2014;9:1385-92. [PubMed]
- Lee JY, Ku BM, Lim SH, et al. The BIM Deletion Polymorphism and its Clinical Implication in Patients with EGFR-Mutant Non-Small-Cell Lung Cancer Treated with EGFR Tyrosine Kinase Inhibitors. J Thorac Oncol 2015;10:903-9. [PubMed]
- Isobe K, Hata Y, Tochigi N, et al. Clinical significance of BIM deletion polymorphism in non-small-cell lung cancer with epidermal growth factor receptor mutation. J Thorac Oncol 2014;9:483-7. [PubMed]
- Zhao M, Zhang Y, Cai W, et al. The Bim deletion polymorphism clinical profile and its relation with tyrosine kinase inhibitor resistance in Chinese patients with non-small cell lung cancer. Cancer 2014;120:2299-307. [PubMed]
- Chen X, Liu H, Xing H, et al. The BIM deletion polymorphism cannot account for intrinsic TKI resistance of Chinese individuals with chronic myeloid leukemia. Nat Med 2014;20:1090. [PubMed]
- Soh S, Ong ST. A novel BIM deletion polymorphism: implications and lessons for cancer targeted therapies. Rinsho Ketsueki 2013;54:1714-9. [PubMed]
- Youle RJ, Strasser A. The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol 2008;9:47-59. [PubMed]
- Adachi M, Zhao X, Imai K. Nomenclature of dynein light chain-linked BH3-only protein Bim isoforms. Cell Death Differ 2005;12:192-3. [PubMed]
- Costa DB, Halmos B, Kumar A, et al. BIM mediates EGFR tyrosine kinase inhibitor-induced apoptosis in lung cancers with oncogenic EGFR mutations. PLoS Med 2007;4:1669-79; discussion 1680.